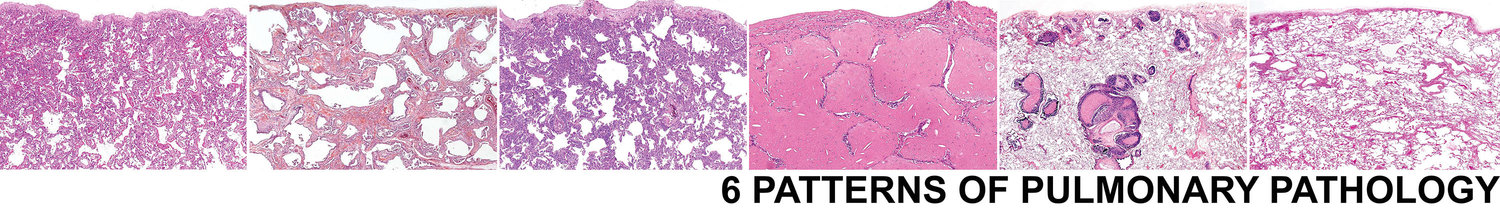
Pattern 4 Alveolar Filling
Basic Elements of the Pattern: Alveoli in the biopsy filled with cells or non-cellular material (Figure 19)
Key Modifiers: With immature fibroblasts, with macrophages, with proteinaceous material, with blood and siderophages, with neutrophils
This pattern of lung disease occurs as a component of a number of different pathological processes such as acute and organizing infections, pulmonary hemorrhage, pulmonary alveolar proteinosis, chronic eosinophilic pneumonia, desquamative interstitial pneumonia, respiratory bronchiolitis-associated interstitial lung disease (RBILD) and many others. Parenchymal consolidation alone is not helpful in the differential diagnosis except when the filling process is distinctive or nearly diagnostic, such as pulmonary alveolar proteinosis (granular proteinaceous material) or chronic eosinophilic pneumonia (pink macrophages, fibrin and eosinophils).
4a. Alveolar filling with immature fibroblasts (OP pattern)
Organizing pneumonia (OP pattern) is a very common reaction pattern in the lung. The presence of intra-luminal tufts of plump fibroblasts and immature connective tissue within alveolar ducts and more distal airspaces has been traditionally referred to as “bronchiolitis obliterans organizing pneumonia” or “BOOP” by pathologists. Today we use the term “OP pattern” as a more generic descriptor of the lesion and to avoid potential confusion with “idiopathic BOOP” (now cryptogenic organizing pneumonia). An OP pattern is especially evident in organizing acute lung injury from any etiology. Organizing pneumonia can be accompanied by alveolar fibrin and/or hyaline membranes if acute injury is ongoing. This morphology typically will be associated with acutely illness, whereas the patient with pure organizing pneumonia pattern will often have a more subacute presentation.
OP is seen in a number of settings (see below), most notably in cryptogenic organizing pneumonia (COP), a form of idiopathic ILD.[31] The most consistent finding in COP is patchy involvement of the airspaces by small tufts of immature fibroblasts distributed within terminal bronchioles, alveolar ducts, and alveoli (Figure 20). Other findings that may accompany an OP pattern include interstitial infiltrates of mononuclear cells, fibrinous exudates, foam cells in the airspaces, and prominent type II pneumocytes. Common causes of an OP pattern are presented in Table 9.
TABLE 9 Common causes of the organizing pneumonia pattern (modified after Leslie, Colby and Swensen[1])
Organizing infections (any cause) Drug and toxin reactions
Organizing diffuse alveolar damage Systemic collagen vascular diseases
Hypersensitivity pneumonitis Eosinophilic pneumonia
Organizing infectious pneumonias in: Airway obstruction
-chronic bronchitis and emphysema Cryptogenic organizing pneumonia
-bronchiectasis Peripheral reaction around:
-cystic fibrosis -abscesses, infarcts, Wegener’s granulomatosis,
-aspiration pneumonia and others
-chronic bronchiolitis
4b. Alveolar filling with macrophages (DIP-like reaction)
A desquamative interstitial pneumonia- like (DIP-like) pattern is characterized by increased numbers of alveolar macrophages, with mild associated inflammatory changes in alveolar walls (Figure 21). Lesions that may show a DIP pattern (in some cases focally) are presented in Table 10.
TABLE10Conditions associated with a DIP-like reaction (modified after Leslie, Colby and Swensen[1])
Obstructive pneumonias (with foamy alveolar macrophages)
Exogenous lipoid pneumonia and lipid storage diseases
Infection in the immunosuppressed patient (“histiocytic pneumonia”)
Respiratory bronchiolitis-associated interstitial lung disease (RBILD)
Pulmonary Langerhans cell histiocytosis
Drug reactions
Chronic alveolar hemorrhage
Eosinophilic pneumonia
Certain pneumoconioses (especially talcosis, hard metal disease, and asbestosis)
Idiopathic DIP
The idiopathic form of DIP described by Carrington represents a distinct pathologic entity that has clinical, radiologic, and prognostic differences from idiopathic UIP.[32] Some cases previously classified as DIP can be reasonably reclassified as “respiratory bronchiolitis-associated interstitial lung disease” (RB-ILD), an interstitial lung disease of smokers that does not appear to progress to advanced fibrosis.[33]
The cytologic features of the macrophages in all of these conditions vary considerably and are helpful at times in pointing to a specific diagnosis. In RB-ILD, the macrophages are airway-centered and contain fine, light-brown, cytoplasmic pigmentation with delicate black punctation, findings characteristic of smokers macrophages. In amiodarone reactions, obstructive pneumonias, lipoid pneumonia, and storage diseases, foamy or vacuolated histiocytes predominate. In hard metal disease (cobalt pneumoconiosis), distinctive multinucleated intra-alveolar histiocytes are the dominant finding.[34] Chronic alveolar hemorrhage is associated with extensive hemosiderin-laden macrophages in the airspaces.[14] The distinctive features of eosinophilic pneumonia are the presence of interstitial and airspace eosinophils, airspace fibrin, markedly reactive type II cells and dense alveolar macrophages.[12] Birefringent material can be identified within the DIP-like reaction in many of the pneumoconioses. Large and small clear spaces, often engulfed by giant cells and associated with variable fibrosis, characterize exogenous lipoid pneumonia (Figure 22).
4c. Alveolar filling with eosinophilic material
The prototype of this pattern is pulmonary alveolar proteinosis (PAP). This distinctive disease results in dense granular eosinophilic material filling adjacent alveoli. PAP can be focal or segmental in distribution. Cholesterol clefts and hyaline globules are typically present in the granular infiltrates and a rim of retraction often separates the infiltrates from adjacent alveolar walls (Figure 23). The disease occurs commonly as a primary idiopathic form, but may also be seen as a secondary phenomenon in the settings of occupational disease (especially dust-related), drug-induced injury, hematologic diseases, and in many settings of immunodeficiency.[35, 36] The granularity of the alveolar material helps differentiate PAP from other alveolar filling processes (such as pulmonary edema and Pneumocystis infection).
4d. Alveolar filling with blood and siderophages
Alveolar hemorrhage syndromes (discussed in Pattern 1d) are the diagnosis of exclusion for this alveolar filling pattern. Sometimes striking alveolar hemorrhage can be seen in urgent lobectomy specimens from patients with persistent hemoptysis related to bronchiectasis or other airway/vascular abnormality. As always, the clinical context is essential, as this is most often a localized (i.e. lobar) phenomenon.
4e. Alveolar filling with neutrophils
Acute infectious bronchopneumonia is the prototype for alveolar filling with neutrophils. This pattern is most commonly identified in autopsy material and rare in surgical biopsies. When this pattern is seen very focally in the biopsy, consider other causes of neutrophil exudation, particularly capillaritis in diffuse alveolar hemorrhage.