6 Patterns > Acute Lung Injury Pattern > Subpatterns > w/ Hayline Membranes > Foreign Material Associated DAD
Foreign Material Associated DAD
…UNDER CONSTRUCTION…
The distinction between infectious and noninfectious causes of DAD is the most important job of the pulmonary pathologist in the setting of an acute lung injury pattern biopsy. For this reason, AFB and GMS stains (often on multiple blocks) are essential components of the work up. In immunocompetent pateints, if the biopsy lacks neutrophils, viral cytopathic effect, granulomas, and necrosis, infection becomes much less likely. However if the patinet is immunsuppressed, any acute lung injury should be considered infectious until proven otherwise.
SEE BELOW FOR SAMPLE SIGNOUT
If you are considering a diagnosis of infectious DAD, the biopsy should show the following features:
Hyaline membranes
Edema
May have focal areas of increased neutrophils, necrosis, granulomas, or viral cytopathic effect
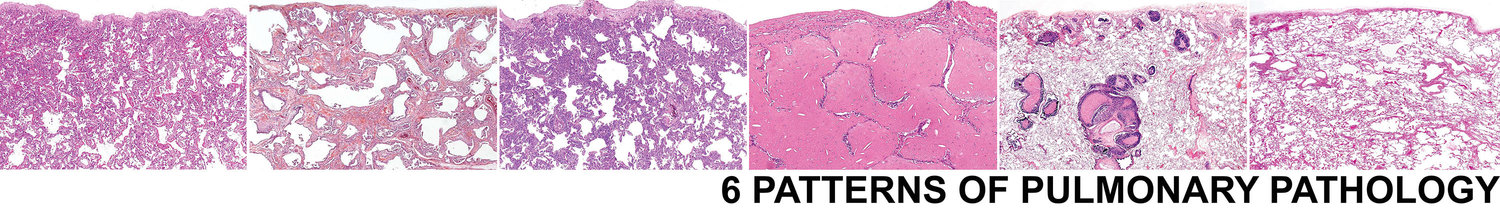
Pink biopsy of ALI from Low Power
Edema
Hyaline Membranes
Necrosis
Granulomas
Neutrophils
Viral Cytopathic Effect
Biopsies with the following features may not be infection associated DAD:
Robust lymphoplasmacytic interstitial inflammation (consider CTD)
Pleuritis (consider CTD)
Lymphoid follicles (consider CTD)
Interstitial giant cells or poorly formed granulomas (consider chronic HP)
Foamy macrophages and type II pneumocytes (consider drug reaction)
Foreign material (consider aspiration or intravenous)
Alveolar hemosiderin laden macrophages and capillaritis (consider alveolar hemorrhage syndrome)
Background fibrosis (consider acute on chronic ILD)
Cellular interstitial inflammation (consider CTD)
Lymphoid follicles (consider CTD)
Foamy macrophages and type II pneumocytes (consider drug reaction)
Alveolar hemosiderin laden macrophages and capillaritis (consider alveolar hemorrhage syndrome)
Pleuritis (consider CTD)
Interstitial giant cells or poorly formed granulomas (consider chronic HP)
Foreign material (consider aspiration or intravenous)
Background fibrosis (consider acute on chronic ILD)
Clinical Presentation
UIP of IPF is a disease of older patients (typically greater than 60)
UIP is much more common in men than women (3 to 1)
Patients present with slowly worsening SOB and caugh
Patients often have a smoking history
There should be no history of autoimmune disease, exposure to organic antigens or occupational exposure
Radiology
Peripheral and subpleural predominant reticulation
Lower lobes more involved than upper lobes
Honeycomb cyst formation
GGO should be absent
No air trapping should be present
Sample Signout
If you are suspicious for an infectious etiology for the ALI biopsy, consider the following approach to signing the case out:
Acute and organizing diffuse alveolar damage with ______(insert necrosis, neutrophils, viral cytopathic effect, and/or granulomas) highly suspicious for an infectious etiology (see comment)
Comment: The biopsy shows an acute and organizing acute lung injury process. The presence of _______(insert necrosis, neutrophils, viral cytopathic effect, and/or granulomas) is suggestive of an infectious etiology. AFB and GMS (and IHC if viral cytopathic effect) stains have been ordered on multiple blocks. Regardless of weather they are positive or not, infection is still favored. Correlation with final culture studies and infectious serologic studies is suggested.
If the the biopsy shows DAD without any additional specific histologic features, consider the following approach:
Acute and organizing diffuse alveolar damage (see comment).
Comment: The biopsy shows acute and organizing diffuse alveolar damage. There is a broad differential diagnosis including infection, drug reaction, CTD, aspiration, and as an idiopathic entity. No additional specific histologic features to indicate an etiology are identified. AFB and GMS stains have been ordered on multiple blocks. If the patient is immunocompetent, the absence of necrosis, neutrophils, viral cytopathic effect, and granulomas makes infection less likely, although it cannot be excluded. The diagnosis of ILD requires a multidisciplinary approach. Correlation with microbiology studies, imaging studies and clinical history is suggested.