6 Patterns > Acute Lung Injury > Subpatterns
Acute Lung Injury Subpatterns
There are 8 subpatterns in the setting of acute lung injury. We use the pneumonic C-DEB-FISH to remember to look for all the causes of acute lung injury.
C = Connective Tissue Disease (lymphoplasmacytic infiltrates, pleuritis)
D = Drug Reaction (foamy cytoplasm in macrophages and pneumocytes)
E = Acute Eosinophilic Pneumonia (eosinophils, fibrin, reactive pneumocytes)
B =Diffuse Alveolar Hemorrhage (blood and capillaritis)
F = Foreign Material (food, embolized material)
I = Infection (necrosis, granulomas, neutrophils, viral cytopathic effect)
S = Background Fibrosing ILD (scarring)
H = Hypersensitivity Pneumonitis (granulomas and cellular infiltrates)
Click the image most similar to your case. It may be okay to see more than one pattern.
w/ Hyaline Membranes
Infection
Drug Reaction
Connective Tissue Disease
Idiopathic (DAD/ARDS)
w/ Eosinophils
Acute eosinophilic pneumonia
Drug Reaction
Infection
DAD in smokers
w/ Granulomas
Infection
Subacute HP
w/ Neutrophils
Infection
Alveolar Hemorrhage Syndrome with capillaritis
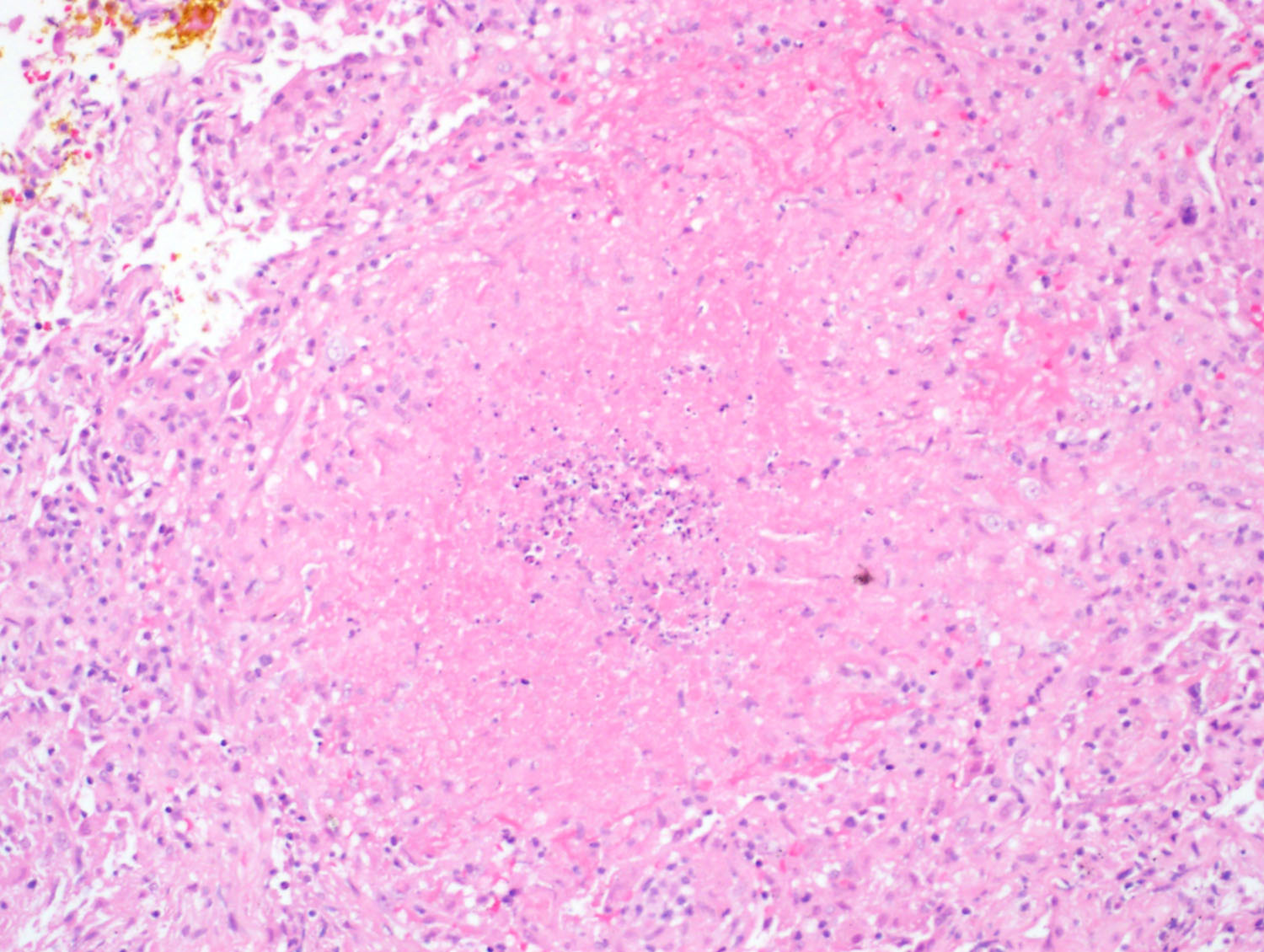
w/ Necrosis
Infection
ANCA-Associated Disease
Infarction
w/ Foreign Material
Aspiration
Embolized Drug/chemo
Silicone pneumonia
w/ Hemosiderin Macrophages
Acute and Organizing Alveolar Hemorrhage Syndrome
w/ Cellular Interstitial Infiltrates
Connective Tissue Disease
Subacute HP
w/ Background Fibrosis
Acute exacerbation of underlying ILD
Sample Signout of the Acute Lung Injury Biopsy
If no additional specific histologic features are identified, consider the following approach to signing the case out:
Acute and organizing lung injury (see comment).
Comment: The biopsy shows acute and organizing lung injury. There is a broad differential diagnosis including infection, drug reaction, CTD, aspiration, and as an idiopathic entity. No additional specific histologic features to indicate an etiology are identified. The diagnosis of ILD requires a multidisciplinary approach. Correlation with microbiology studies, imaging studies and clinical history is suggested.