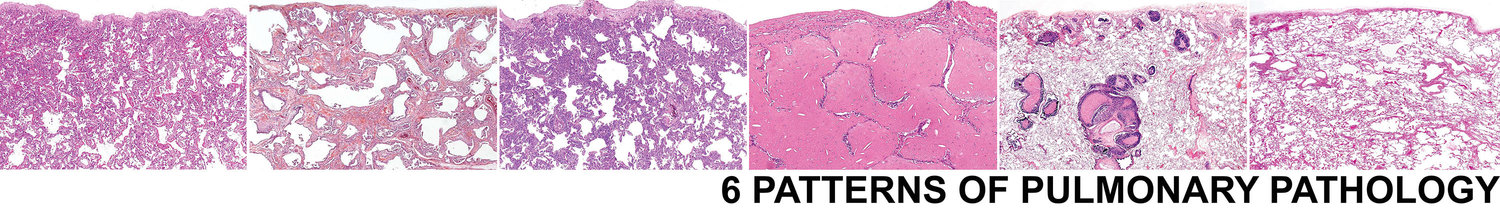
6 Patterns > Fibrosis Pattern > Additional Features > w/ Variable Involvement > Connective Tissue Disease
Connective Tissue Disease-Associated Interstitial Fibrosis
The fibrosis seen in the setting of CTD-ILD can vary dramatically from a UIP patient to an NSIP pattern. Many cases will show an overlap with some areas looking very good for NSIP wile other areas look like NSIP. Active injury in the form of fibroblast foci are common (up to 20% of cases). Areas of extensive architectural distortion and honeycomb remodeling is also common (up to 20% of cases). The histologic hallmark of CTD-ILD fibrosis is a robust lymphoplasmacytic infiltrate. These biopsies should look blue from low power.
SEE BELOW FOR SAMPLE SIGNOUT
If you are considering a diagnosis of CTD-ILD, the biopsy should show the following features:
Pulmonary fibrosis with a UIP, NSIP, airway centered, or mixture of patterns.
Marked lymphoplasmacytic infiltrates
Lymphoid follicles, including secondary follicles
Pleuritis
UIP pattern fibrosis in CTD
NSIP pattern fibrosis in CTD
Marked lymphoplasmacytic infiltrates
Pleuritis
Lymphoid follicles
Biopsies with the following features should raise concern for alternative etiologise:
Areas of completely normal lung (consider UIP of IPF)
Sharp demarcations between advanced fibrosis and normal lung (consider UIP of IPF)
Numerous giant cells, especially if in the interstitium (consider chronic HP)
Granulomas (consider chronic HP or Sarcoid)
Abundant dust and inhalational debris (consider pneumoconiosis)
Areas of normal lung (consider UIP)
Granulomas (consider chronic HP or Sarcoid)
Sharp demarcations (consider UIP)
Numerous giant cells, especially if in the interstitium (consider chronic HP)
Abundant dust and inhalational debris (consider pneumoconiosis
Clinical Presentation
CTD-ILD is more common in female patients and those how are younger. Great caution should be taken if diagnosing UIP in a female younger then 60.
Patients present with slowly worsening SOB and caugh
Up to 20% of patients with pulmonary manifestations of CTD may present with respiratory symptoms prior to other clinical and/or serologic evidence of CTD
There should be no history of exposure to organic antigens or occupational exposure
Radiology
The radiology appearance depends on the patterns of fibrosis present. Peripheral and subpleural predominant reticulation with honeycombing may be present, mimicking UIP
GGO and infiltrates should may be present, depending on the amount of NSIP and OP present in the biopsy
Air tripping may be present
Sample Signout
If you are comfortable that the biopsy has features of CTD-ILD, consider the following approach to signing the case out:
Advanced fibrosing interstitial pneumonia with marked lymphoid hyperplasia and pleuritis. An as yet to be fully elucidated CTD leads the differential diagnosis (see comment)
Comment: The biopsy shows advanced fibrosis with marked lymphoid hyperplasia and pleuritis. There is patchy superimposed organizing pneumonia. These features are suggestive of a CTD-ILD. Correlation with a clinical and extensive work up for CTD is suggested.
Reference:
Practical Pulmonary Pathology: A diagnostic Approach, 3rd Ed. Page 247.