6 Patterns > Fibrosis Pattern > Additional Features > w/ Acute Lung Injury
Fibrosis w/ Acute Lung Injury
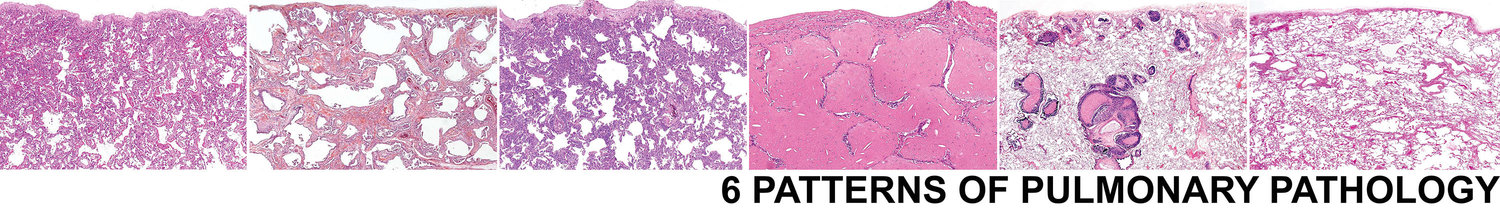
Biopsies showing both acute lung injury and fibrosis are some of the most challenging cases. However, a simple approach is to characterize the acute component (fibrin, OP, DAD) and the chronic component (UIP, NSIP, airway-centered) individually. There are 4 main settings this pattern is seen in, acute exacerbation of UIP, flare of CTD, subacute on chronic HP, and acute on chronic aspiration.
Acute Exacerbation of Usual Interstitial Pneumonia
Background fibrosis should have peripheral and subpleural distribution typical of UIP.
Should have numerous fibroblast foci or other features of acute lung injury
"Normal" areas will be involved by acute lung injury (note the fibrin between the green dots and the reactive pneumocytes)
Acute on Chronic Aspiration
Foreign material
Food
Polarizable material
Flare of Connective Tissue Disease
Often with a more "blue" appearance due to inflammatory cells.
Areas of cellular interstitial inflammation similar to cellular NSIP.
Lymphoid follicles with germinal centers
Pleuritis
Follicular bronchiolitis
Subacute on Chronic Hypersensitivity Pneumonitis
Should show giant cells and poorly formed interstitial granulomas.
Sample Signout
If no additional specific histologic features are identified, consider the following approach to signing the case out:
Acute on chronic interstitial lung disease (see comment).
Comment: The biopsy shows histologic evidence of both acute and chronic ILD. The predominant pattern of the acute component is _______ (select OP, DAD, fibrin, etc). The predominant pattern of the chronic compoennt is ______ (select UIP, NSIP, airway-centered, etc). No additional specific histologic features to indicate an etiology are identified. There is a broad differential diagnosis including acute exacerbation of UIP, flare of CTD, subacute on chronic HP, and acute on chronic aspiration. The diagnosis of ILD requires a multidisciplinary approach. Correlation with imaging studies and clinical history is suggested.